Epilepsy, a baffling neurological enigma, manifests as spontaneous seizures arising from unanticipated cerebral electrical tumult. Children’s seizures adopt diverse guises – transient vacant gazes to all-encompassing convulsions. Singular episodes may punctuate one child’s life while others grapple with incessant occurrences necessitating continuous treatment and management. Comprehending seizure variations and their potential reverberations on a child’s health and growth trajectory is crucial for parents and caregivers.

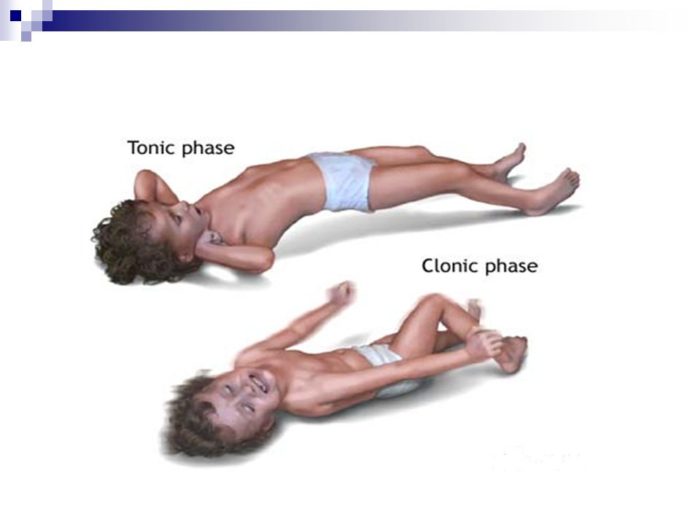
A myriad of seizure types besiege children: focal (partial), generalized, febrile seizures each with unique characteristics. Focal tempests stem from singular brain locales, inciting twitching or peculiar sensations restricted to one bodily hemisphere. Generalized fits engulf both cerebral hemispheres simultaneously, culminating in either consciousness loss or muscular rigidity followed by rhythmic spasms known as convulsions. Febrile paroxysms exclusively afflict younglings due to precipitous body temperature elevation often induced by infection or illness.
Efficacious epilepsy management hinges upon early detection through vigilant monitoring of telltale signs such as involuntary motions, behavioral fluctuations or awareness alterations alongside post-episode confusion or disorientation. The repercussions vary per child influenced by factors like frequency, severity, root causes underpinning the condition alongside suitable medical intervention/support throughout this journey; nevertheless it remains vital that families collaborate intimately with healthcare professionals ensuring optimal outcomes remain attainable despite the tribulations posed by an existence marred by epilepsy\n
Types of Seizures: Focal, Generalized, and Febrile
Seizures, a bewildering phenomenon, may be categorized into three enigmatic types: focal, generalized and febrile. Focal seizures arise when bizarre electrical activity remains limited to one peculiar area of the brain. Symptoms in this cryptic category vary based on the affected region – involuntary muscle movements, alterations in sensation or perception and even shifts in consciousness might occur. In contrast, generalized seizures engulf both sides of the brain simultaneously, typically causing loss of consciousness alongside rhythmic muscle contractions. Febrile convulsions are an oddity; they specifically target young children aged six months to five years and are triggered by high fever without necessarily signifying epilepsy.
Discerning the signs that a child is experiencing a seizure is vital for prompt intervention and apt care management. Common symptoms include sudden jerking movements or stiffening muscles; staring spells or unresponsive periods; rapid eye blinking or rolling eyes upwards; inexplicable sensations such as tingling feelings or smelling strange odors sans apparent source. It’s worth noting that certain medical conditions can masquerade as seizures but aren’t truly epileptic events – hence it’s crucial for parents to consult healthcare professionals if their child exhibits worrisome behavior.
While concrete reasons behind recurring seizures (i.e., those diagnosed with epilepsy) remain elusive in children who experience them often various factors could trigger individual occurrences – stress levels fluctuating blood sugar levels sleep deprivation exposure to specific substances bright flashing lights etcetera . Should your child potentially undergo any type of seizure – be it focal generalized febrile – seeking professional advice from doctors adept at diagnosing managing treating epilepsy-related disorders becomes essential so they can offer precise assessments tailored treatment options best suited needs ensuring optimal quality life despite challenges posed living condition\n
Recognizing the Signs and Symptoms of Seizures in Children
Discerning the indications and manifestations of seizures in youngsters is critical for prompt interference and suitable administration. Seizures can materialize in an assortment of ways, contingent upon the type of seizure encountered by the little one. Focal seizures, likewise known as partial seizures, transpire when anomalous electrical movement influences just a single side or part of the cerebrum. Side effects may incorporate involuntary motions or convulsions on one side of the body, abrupt changes in feelings or impressions, and adjustments in visual or auditory perception.
In contrast, generalized seizures encompass both sides of the brain concurrently and are typified by a loss of cognizance, muscle rigidity, and spasmodic movements.
A further prevalent kind of seizure among juveniles is absence seizures which exhibit distinctively from focal and generalized seizures. These occurrences typically endure only a few seconds but can be effortlessly disregarded since they frequently manifest as concise staring spells with no noticeable physical manifestations. It is crucial to acknowledge that some children might undergo multiple various types of seizures all through their lives due to fluctuating triggers such as elevated fever or unprovoked reasons leading them to develop epilepsy.
Guardians ought to acquaint themselves with these unmistakable appearances so they can rapidly recognize if their youngster is experiencing a seizure scene. Besides this, it’s imperative to keep track any patterns linked with these occasions – like explicit triggers – so fitting preventive measures can be executed progressing forward. Early acknowledgment not exclusively helps immediate treatment but also aids in minimizing possible long-term impacts on advancement while guaranteeing better overall care for affected children\n
Causes and Triggers of Seizures in Young Ones
In the realm of childhood seizures, myriad factors contribute to their onset, necessitating a thorough comprehension for parents and caregivers seeking efficacious treatment. Among these multifarious causes are genetic predispositions, cerebral anomalies or traumas, infections plaguing the central nervous system, metabolic disorders, and specific medications. Occasionally, pinpointing an exact origin proves elusive; it is vital to note that not all seizures signal epilepsy—though recurrent unprovoked episodes often culminate in such a diagnosis.
Discerning potential instigators of a child’s seizures paves the way for prevention and enhanced management. Varied seizure types—myoclonic (fleeting muscle jerks), convulsive (shaking or stiffening), atonic (abrupt loss of muscle tone), tonic (muscle rigidity) and febrile convulsions (fever-related)—share common triggers: sleep deficit, stress or anxiety, flashing lights or patterns and sudden temperature shifts accompanying fever-induced febrile convulsions. Furthermore, particular illnesses may heighten symptoms preceding seizure occurrences.
When monitoring children for seizure indicators, guardians must remain vigilant regarding each type’s distinct attributes: myoclonic-astatic epilepsies entail transient lapses in muscle tone succeeded by falls; absence epilepsies materialize as unresponsive staring spells; complex partial epilepsies encompass disorientation alongside repetitive behaviors such as lip-smacking during episodes—all uniquely disparate yet demanding swift attention when detected early on. This enables timely interventions upon extensive evaluation from skilled professionals who specialize in personalized pediatric neurology care services based on clinical presentation discerned throughout comprehensive assessment processes designed to ultimately optimize therapeutic outcomes achievable via targeted intervention strategies executed accordingly upon establishment of definitive diagnoses rendered conclusively thereby facilitating optimal patient care management overall.
Diagnosing Seizures: Tests and Evaluations for Children
A labyrinthine endeavor it becomes, the diagnosis of seizures in young ones, given the myriad manifestations they exhibit. To pinpoint an accurate diagnosis for your offspring’s ailment, thorough documentation of their seizure episodes must be conveyed to medical experts. Particulars such as duration, probable instigating factors, and symptoms witnessed during each occurrence are vital pieces of information. It is crucial for guardians to comprehend that variations may arise in these presentations based on whether the child experiences epilepsy-induced seizures or those resulting from other conditions like fever-related (febrile) convulsions or provoked incidents.
Further complications emerge in discerning epilepsy when a juvenile encounters complex febrile seizures or manifold types of epileptic events. Atonic seizure – characterized by abrupt loss of muscle tone leading to uncontrolled falling or head drooping without losing consciousness – remains one predominant form experienced by children. Other classifications encompass tonic-clonic (formerly grand mal), absence (petit mal), myoclonic, and focal onset impaired awareness (complex partial). Each bears its own unique symptomatology; for instance, solely atonic seizures manifest with loss of muscle tone while vacant staring spells typify absence variants.
In pursuit of accuracy regarding diagnoses and comprehending why diverse forms materialize among younger patients, physicians often employ an array tests and evaluations including electroencephalograms (EEGs) – brain activity measurements – alongside magnetic resonance imaging (MRI) scans aimed at detecting structural anomalies within cerebral tissue itself. Additionally conducted may be blood examinations seeking to eliminate metabolic disorders or infections potentially inciting non-epileptic provoked
seizures . By exhaustively scrutinizing all plausible contributing elements via these diagnostic instruments and assessments , healthcare specialists find themselves better prepared not merely for identifying which type(s) but also determining suitable treatment plans crafted specifically according individual necessities circumstances encircling each case.\n
Treatment Options: Medications and Therapies for Seizure Management
The paramount objective in addressing the conundrum of seizures amongst juvenile individuals is the meticulous regulation and tempering of said incidents, thereby augmenting their existential satisfaction. Upon identification of such convulsive events, medical practitioners commonly advocate for antiepileptic elixirs designed to thwart or mitigate recurrent seizure manifestations. The selection of these potions hinges on a myriad of elements, encompassing the variety and intensity of the young one’s affliction, chronological development, plausible adverse reactions, and interplay with additional medicinal concoctions. Adherence to prescribed therapeutic strategies whilst maintaining unwavering contact with health guardians is indispensable for achieving prime seizure governance.
Beyond chemical prophylaxis lies an assortment of non-pharmacological remedies that may prove advantageous for youth beset by seizures. Instances abound where maturation rescinds a child’s inclination towards seizures; under scrupulous oversight, physicians might contemplate progressive diminution or cessation thereof medicaments in such situations. Nutritional tactics – exemplified by ketogenic regimens – demonstrate potential efficacy in tackling drug-defiant epilepsy amid younger and older populations alike; notwithstanding this promise, implementation ought only proceed under specialist counsel given inherent perils entwined with rigorous dietary limitations. Moreover, apparatuses like vagus nerve exciters contribute to seizure attenuation via transmission of electrical stimuli through cervical nerves directly interfacing cerebral zones implicated in epileptic phenomena.
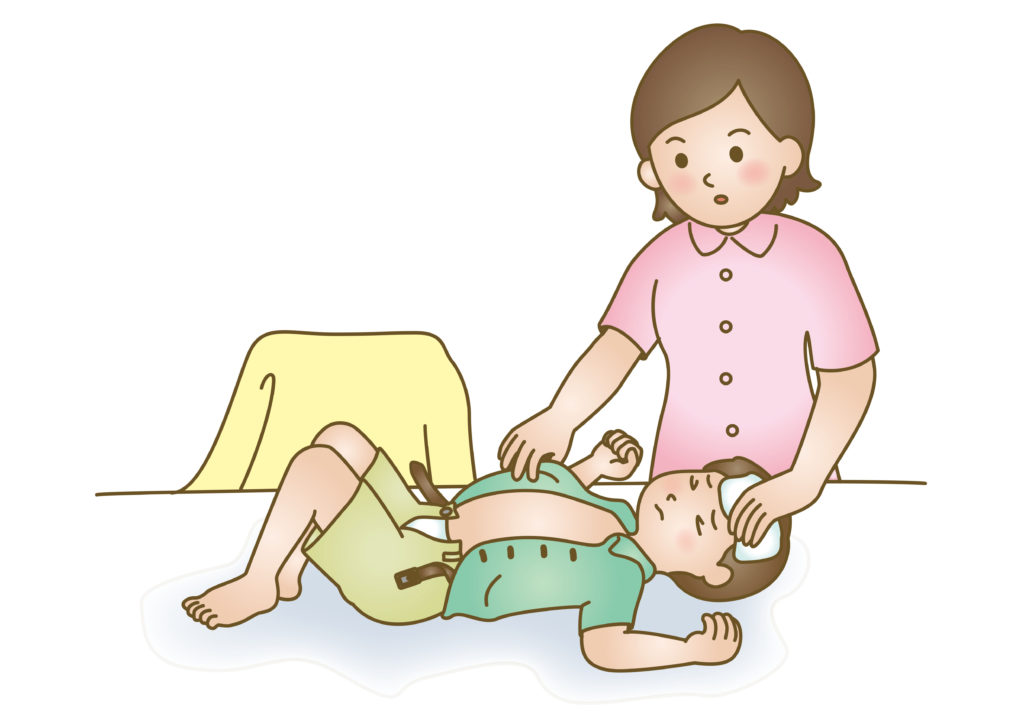
It remains imperative that progenitors and custodians acquire proficiency in discerning indicators presaging seizures so as to proffer fitting succor during a child’s convulsive event. Amidst episodes typified by abrupt spasmodic motions or lapses into unconsciousness (e.g., generalized tonic-clonic convulsions), constraining juveniles must be eschewed; rather their security should be prioritized through lateral repositioning away from lurking dangers until spasms ebb organically – customarily within minute spans. Subsequent thereto an episode conclusion may find them fatigued or bewildered; proffering solace and permitting repose will expedite recuperation with greater efficacy than precipitous resumption of quotidian undertakings following an event.
Helping Your Child Cope with Seizures and Their Effects
Grasping the multifarious seizure categories is paramount for assisting your offspring in navigating epilepsy and convulsive disorders. Diverse general seizures, such as absence, atonic, myoclonic, and tonic-clonic are not uncommon. The former almost exclusively commences during juvenility and manifests as fleeting interruptions in awareness or fixed gazes. Atonic seizures entail an abrupt depletion of muscle rigidity which often precipitates falling. Myoclonic seizures encompass sudden spasms of limbs while tonic-clonic seizures primarily transpire as full-body convulsions.
Apprehending the timing of seizure occurrences can prove advantageous in regulating their impact on your progeny’s quotidian existence. For example, some young ones may undergo heightened frequency of these episodes within a day following fever inception or due to specific instigators like inadequate slumber or exposure to pulsating luminosity. Recognizing such prevalent triggers empowers parents to employ tactics that mitigate their incidence or intensity for their offspring.
Moreover, comprehending your child’s seizure variety and possible catalysts necessitates investigating the plethora of treatment alternatives obtainable for epilepsy control. Various medications effectively address seizures; however, pinpointing the optimal pharmaceutical blend may require time via experimentation under medical oversight. Other non-drug-related interventions involving dietary adjustments (e.g., ketogenic diet) or apparatuses (e.g., vagus nerve stimulator) could be contemplated depending on personal requisites and predilections as well. Collaborating closely with healthcare practitioners specializing in juvenile neurology or epileptology services enables families to devise all-encompassing care schemes tailored explicitly towards managing their child’s distinct epilepsy manifestations while minimizing adverse consequences from treatments involved
Prevention and Safety Measures for Children with Seizure Disorders
In the perplexing realm of seizure management for children, grasping the numerous elements inciting such events is of paramount importance. Indeed, certain occurrences or circumstances might provoke seizures despite their resemblance to the convulsions themselves. Sleep deprivation, stress, fever and specific medications stand as potential triggers in individuals with epilepsy. Thus, it becomes crucial for parents and caregivers to pinpoint those situations eliciting their child’s seizures in a bid to prevent them. Furthermore, enlightening family members and friends frequently interacting with the child about vital information regarding seizures proves essential.
A plethora of symptoms manifest during seizures in infants and young children depending on the type experienced. Febrile convulsions are common among 6-month-olds up to 5-year-olds due to high fevers; however frightening they may be for first-time witnessing parents, these episodes tend to pose no danger. Though nearly all children outgrow febrile seizures by age six without long-term repercussions or later-life epilepsy development around five percent will experience more episodes throughout childhood. Notably, febrile seizures can span from mere seconds up until several minutes but seldom result in serious complications.
Amid instances where two or more unprovoked convulsions have been diagnosed within short intervals (typically less than six months apart), increased vigilance should ensue when addressing recurrent episode histories involving infants and young children alike. Parents must remain watchful during activities like swimming or bathing wherein water poses heightened risk factors owing to its capacity of conducting electricity through the brain potentially causing further damage if not supervised adequately while engaging alongside their offspring in these activities together with their child’s medication schedule warrants strict monitoring since missed doses could trigger additional cycles leading back into further convulsive experiences.
It remains imperative not only remembering that during a seizure event a child may lack any recollection but also providing solace post-episode offers invaluable assistance coping with their condition